CIPHER BRIEF REPORTING — On September 17th, 1945, just weeks after the Japanese surrender that marked the end of the Second World War, a Connecticut Congresswoman gave a speech that seemed capture the sentiment of a war-weary nation. Every lawmaker, said Rep. Clare Boothe Luce, has been “under constant and terrific pressure from servicemen and their families” to bring the troops home.
Millions of American men and women, dispersed across four continents, had survived the deadliest conflict in human history. Now, it was time for most of them to return to civilian life.
But the process would not be a quick one, carried out mostly by ship, which could take weeks, or even months, depending upon the location of deployment. And yet during those voyages, in which there was often little to do but play cards and perhaps reflect on the years (and traumas) of war, occasionally something interesting also happened.
“They might have had 30 days in the troop ship where they were surrounded by each other and they got to work through their issues together,” explained former acting U.S. Defense Secretary Chris Miller. “They realized, ‘oh, maybe I’m not the only one that’s experienced that.’”
Today, that gradual reintroduction into civilian life, which began aboard those ships amidst a community of peers – and coincided with an era when military suicide levels were at all-time lows – has dramatically sped up by way of modern advances in transportation.
“Talk about cognitive dissonance,” added Miller, who took part in combat operations in Afghanistan in 2001 and Iraq in 2003, as well as several follow-on deployments. “I leave [the battlefield] on July the third, I am sitting in my home for fireworks 12 hours later,” he explained. “You’re fighting for your lives,” and then “here I am with my family at home.”
“I couldn’t help but imagine if I didn’t have the support structure … where I got to do after action reviews, debriefings, and talk to people about it,” he added.
Veterans are generally at higher risk for suicide than the general population, with an average of 17 suicide deaths per day, according to the Centers for Disease Control and Prevention (CDC). They, according to a recent Department of Veterans Affairs report, confront a more than 57% greater suicide rate than non-veteran adults. And over the past two decades, the issue has become particularly pronounced.
Between 2001 and 2019, the rate of suicide among veterans swelled by nearly 36%, compared to an increase of 30% in the general population. Taken collectively, U.S. military deaths by suicide are far higher than the number of Americans killed on the battlefields of Iraq, Syria, and Afghanistan combined.
Looking for a way to get ahead of the week in cyber and tech? Sign up for the Cyber Initiatives Group Sunday newsletter to quickly get up to speed on the biggest cyber and tech headlines and be ready for the week ahead. Sign up today.
A complex and often multifaceted phenomenon, combat exposure and the resulting onset of post-traumatic stress are often thought to be prime suicide culprits among veterans populations. And yet in a wide-ranging study that analyzed Army records from the 1840s to 2017, published in JAMA Network Open and widely considered among the most extensive accounts of veterans’ suicide in the nation’s history, researchers uncovered that suicides were not always directly correlated with combat. A subsequent write-up published in the Journal of the American Medical Association’s JAMA Psychiatry found that suicide attempts in fact peaked around “a time of return home and changing anticipation of deployment length.”
Subsequent reviews revealed that among those struggling upon returning home, medical attention is often in short supply, depending on location, while firearm access is often readily available among veterans more generally.
A separate 2023 JAMA study of nearly 40,000 service members found that more than 1 in 3 service members who participated in TRICARE (the military’s health care program) lived in regions that had no, or very few, military or civilian psychiatrists. “Beneficiaries in low-income communities with high income inequality and rural communities,” study noted, “had the highest likelihood of experiencing a shortage of psychiatrists.”
Simultaneously, veterans, especially in rural communities, anecdotally cite social isolation, loss of mission, and a lack of peer networks as among root causes of mental health conditions, such as anxiety and depression.
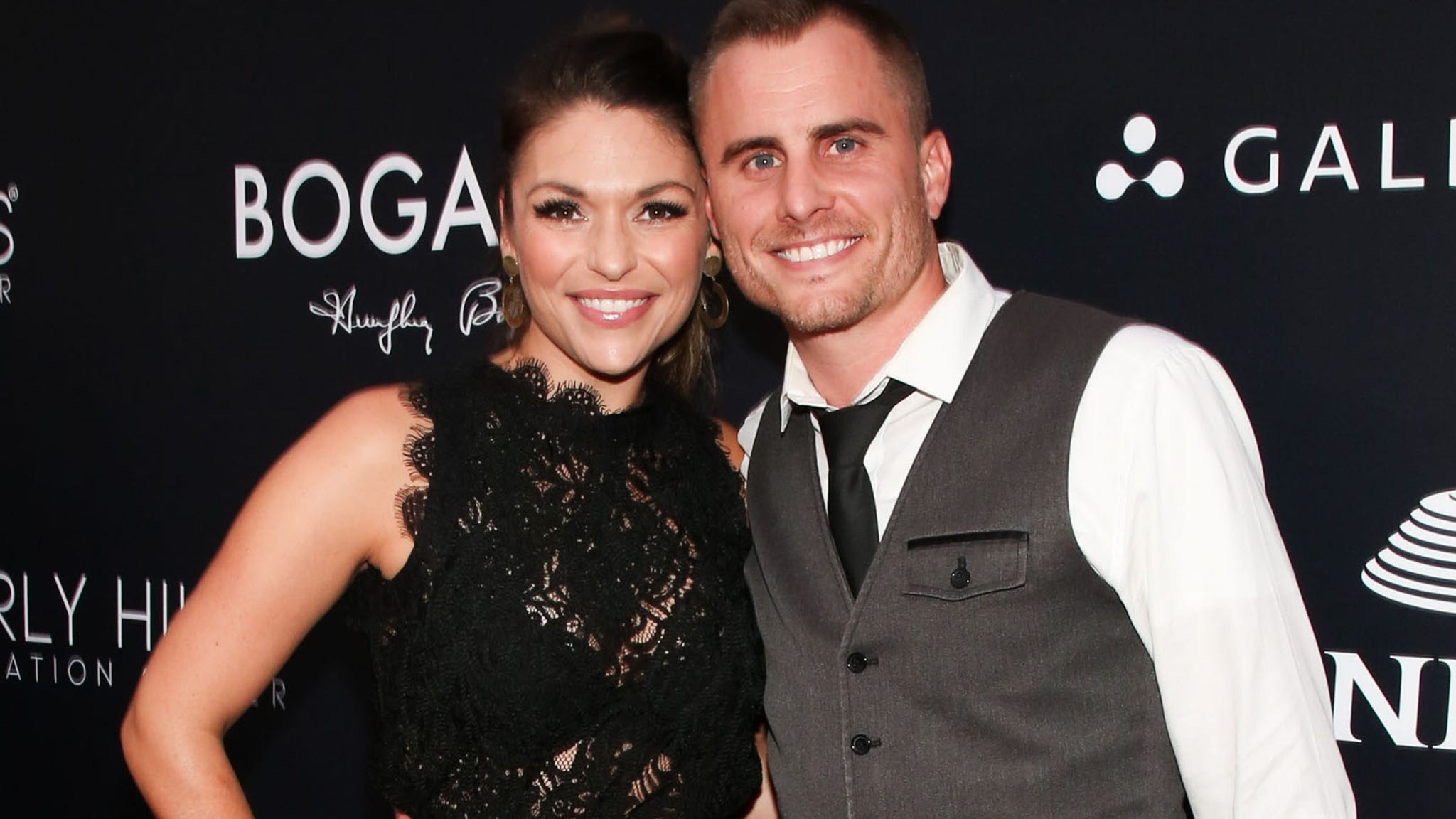
Those factors apparently applied to Michael Carmichael, CW4 Special Forces (retired), who deployed on multiple tours to Afghanistan, Iraq, Syria, and other locales, before retiring from the 5th Special Forces Group (A) in December of 2015.
“I really had anxiety,” he said in an interview with The Cipher Brief. “When my phone would ring, I didn’t even want to look to see who it was, because I didn’t want to answer it.”
The Montana native was living on a military pension on a houseboat in Kentucky. And yet following his last deployment, he described himself as drawing inward.
“You lose your identity,” he said. “You lose your sense of purpose, and … you’re no longer part of a team.”
“Eventually my neighbors took notice,” added Carmichael, now founder and president of the non-profit Check A Vet program — an organization of which former Defense Secretary Miller is on the board — meant to establish peer-to-peer support groups for veterans, employing sponsor models akin to Alcoholics Anonymous (AA).
The Cipher Brief hosts expert-level briefings on national security issues for Subscriber+Members that help provide context around today’s national security issues and what they mean for business. Upgrade your status to Subscriber+ today.
“I wasn’t there in the [community] circle anymore,” he added.
A few of his neighbors then stopped by his home.
“When’s the last time you showered?” one asked, Carmichael recalled. “You stink. Are you going to clean this place up?”
“That was the tough love,” he explained. “But then there was also love, love. And they would take me out on the lake, and we’d go cruise on the pontoon boat somewhere for lunch. And that was great. That was a meaningful and routine relationship.”
That sense of community, Carmichael explained, became the foundation of his broader peer-to-peer suicide prevention effort — a method of which a growing body of research supports.
In fact, a 2015 study published in Oxford University Press revealed the benefits of peer-supported programs in mitigating the effects of veteran suicide, including “social support, purpose and meaning, normalization of symptoms and hope, and therapeutic benefits.”
The report also found that veterans recognized ways in which “peer support could complement psychotherapy for PTSD by increasing initiation and adherence to treatment and supporting continued use of skills after termination.”
“It’s got to be locally-based,” noted former Secretary Miller. “It’s got to be community-based. Not some top-down [approach].”
If you or someone you know is in crisis, call the National Suicide Prevention Lifeline at 800-273-8255, text HOME to 741741.
Read more expert-driven national security news, analysis and opinion in The Cipher Brief because National Security is Everyone’s Business